I used to joke with my friends about having a “food baby” after a meal — when you feel so bloated that it looks as if you’re six months pregnant. But if you also suffer from chronic stomach issues like bloating, gas, and indigestion, you know exactly how un-funny the situation is.
Belly bloat sometimes forced me to stay curled on the couch in a fetal position, and more than a few times, the discomfort even had me limping over to urgent care. These tummy symptoms had a negative impact on my life, and the fact that my gastroenterologist chalked it up to classic IBS (a.k.a. Irritable Bowel Syndrome, which seems to be a blanket diagnosis whenever your digestive symptom flares up), it felt super discouraging that I couldn’t figure out the cause.
I know I’m not alone: In the U.S., gastric discomfort affects between 25 and 45 million people of all ages and genders, but mostly women. When you consume something that you’re sensitive to, it might not only cause you to have IBS-like symptoms (such as bloating), but you might also experience fatigue, headaches, depression, or even an effect on your skin (like dryness or itchiness). It’s difficult to nail down which ingredients you’re reactive to, because of all the many different types of ingredients we consume on a daily basis.
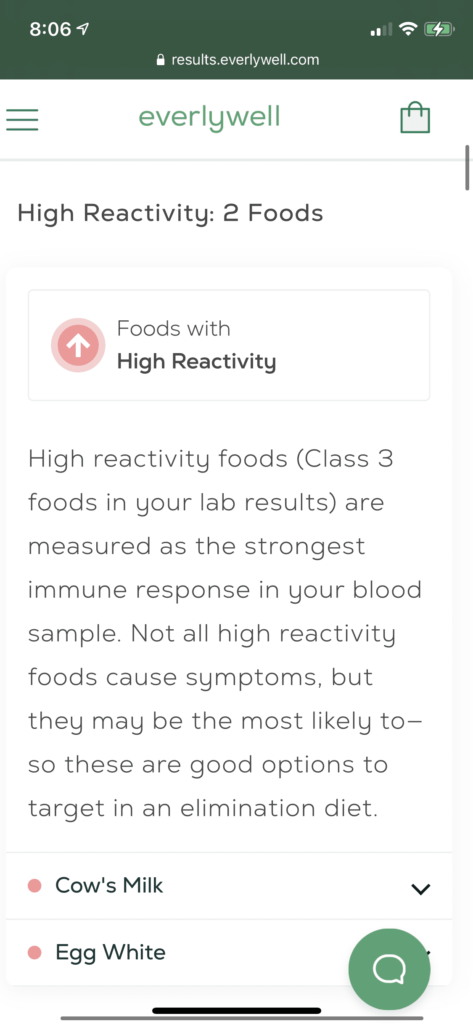
So, are we simply destined to have chronic stomach issues? Maybe not, according to EverlyWell, a recent food sensitivity test I tried. I was served an ad on Instagram — I’m sure thanks to numerous late nights Googling my symptoms. While I went into the process a little dubious (“what could this at-home kit tell me that a doctor couldn’t?”), I ended up learning a lot about what makes my digestive symptom tick. If you want a better understanding of food sensitivities or intolerances, plus how a temporary elimination diet could solve your chronic tummy troubles, let’s dig in:
What’s “food sensitivity” first of all?
Food sensitivity is an overarching term that covers a negative reaction to digesting food and can involve measuring an antibody called Immunoglobulin G (IgG). This is different from food allergies, which are mediated by immunoglobulin E (IgE) antibodies. “Unlike a food allergy, symptoms related to a food sensitivity may be delayed for up to a few days after ingesting the trigger food. A food allergy, on the other hand, may involve life-threatening symptoms and occur shortly after the trigger food is eaten. If you suspect you may have a food allergy, it’s best to consult with an allergist instead of attempting an elimination diet. Food intolerance happens when the body doesn’t produce enough of an enzyme needed to digest a certain food, triggering a rapid, gastrointestinal response. An example of this would be lactose intolerance,” says Sheena Batura, a registered dietitian at EverlyWell.
How can a food sensitivity test help?
Especially with so many doctors’ offices being less accessible for in-person visits over the past year and the struggle to keep up with work and life during a pandemic, a lot of peoples’ diets have gone in a downward spiral. “We saw major upticks in demand for many of our tests during the pandemic, including this one,” says Batura. “It has continued even after doctor’s offices have started offering normal services again. We attribute this to more adults discovering convenient alternatives to things they thought they had to do in person before — along with this mentality of taking control of one’s own health in such a year of uncertainty,” she says. An at-home kit like EveryWell can be done in the comfort of your own home to measure your IgG antibody responses (a.k.a “reactivities”) to figure out what foods are having a negative impact on your well-being.
This particular test that I tried measured my bodies’ IgG immune response to 96 different foods (gluten, dairy, various nuts, meats, fruits, and veggies). The goal is to then use those results to guide an elimination diet plan, which will save you more time and effort from a more extensive and time-consuming elimination diet like FODMAPs.
Who’s the best candidate for this kind of test?
“This test measures the body’s IgG reactivity to 96 foods, such as eggs, several varieties of cheese, ten grains, meat, seafood, spices, vegetables, nuts and more. People who experience headaches, migraines, bloating, stomach or abdominal pain, indigestion and gastrointestinal distress might want to consider taking the test. While there are numerous potential causes for these symptoms, testing the body’s IgG reactivity to these foods and selecting those with elevated reactivities as frontrunners for a temporary elimination diet and the add-back challenge is an excellent place to start,” says Batura.
How does it work?
After I scored it on sale for $127, I received my at-home kit (no doctor’s visits!) and first had to register it online to link my test results to my account. This test required a blood sample and included two lancets to prick your finger to leave a few drops of blood on the collection card. I was lucky that the kit included two lancets, because the first time I tried to prick my finger, I must have not done it deep enough or perhaps my left hand had less blood circulation than my right. Whatever the case, the second time was the charm using my right hand, and I was able to collect enough blood for the sample. I get a bit woozy with anything that has to do with blood, but this wasn’t a big deal at all. It’s significantly less blood than what a traditional laboratory would need. EverlyWell uses a testing method called “dried blood spot,” which requires very little blood, but is just as accurate as what your in-person doctor would use.
Once you seal your sample in a biohazard bag, you slap on the prepaid shipping label, and it’s off for analysis. Because of shipping delays, it took longer than normal to get to their facilities (just about two weeks), and once it was at the lab it took about seven business days to process and for one of their physicians to review the results.
How do you interpret the results?
Your food sensitivity test results tell you how strong your immune system reacts to different foods — based on measurements of IgG antibodies in your blood. Each food is rated on a scale of “0-3,” where “0” is normal and “3” is high reactivity.
- My class 3, “high reactivity” foods – ingredients that had the strongest immune response in my blood sample — included cow’s milk and egg whites.
- My class 2, “moderate reactivity” foods included: almonds, cashews, egg yolks, gluten, mozzarella, rye, wheats, and yogurts.
- My class 1, “mild reactivity” foods included: apples, asparagus, baker’s yeast, barley grains, bell peppers, brans, brewer’s yeast, carrots, chicken, eggplant, garlic, ginger, green beans, green peas, iceberg lettuce, kale, lamb, lemon, soybeans, turkey, white mushrooms, and white potatoes.
- I had 64 foods with “normal reactivity” — a lot of foods that I didn’t even think about.
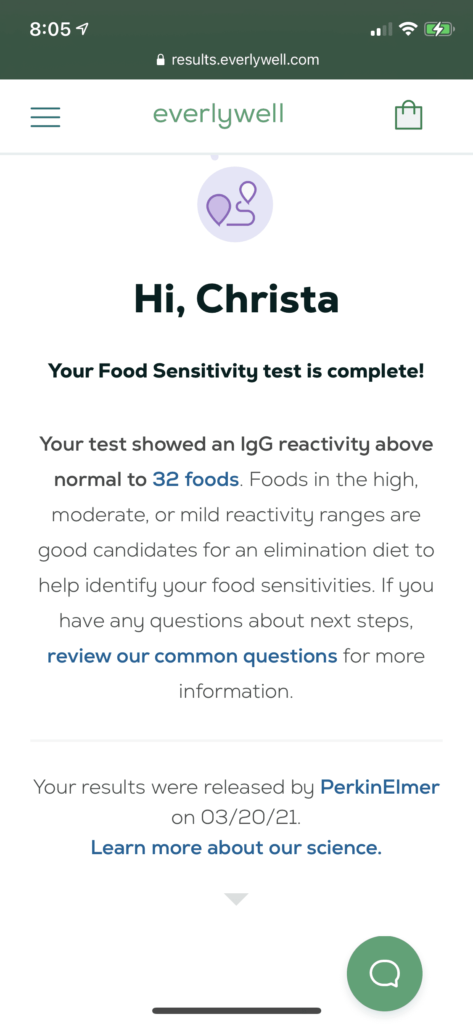
“One important thing to note is that IgG reactivity does not automatically equate to sensitivity. This test does not diagnose food sensitivities; rather, it measures a specific immune reaction that allows you to see which foods might be good candidates for a temporary elimination diet. Many customers report that eggs, cow’s milk and gluten appear high on the list of reactive foods,” says Batura. (I was three for three with the top culprits!)
Another important factor to note is that the ingredient needs to be in your system within the last six months for it to show up on your food sensitivity test. For instance, if you already know that you’re gluten-intolerant and you’ve been religiously avoiding gluten for a while, it’s possible that your IgG antibodies in your sample won’t be elevated for gluten. It can only look for the IgG immune response if the food is already in your system.
I wasn’t surprised by any of my class 1 or 2 results — I eat dairy on a regular basis. I was, however, shocked about ingredients that I don’t eat (like lamb) or some of the “normal reactivity” foods like cod and sunflower seeds that I seemingly haven’t eaten in ages. It turns out unexpected results like these can be hidden in foods (especially pre-packaged foods, cross-contaminated food from a restaurant, or supplements), so it was certainly interesting to see that I never know exactly what I’m consuming.
Soon after I received my test results, I was invited to an optional group Zoom meeting with a dietician to learn more about food sensitivities and go to ask questions on how to interpret my results.
What’s the point of the elimination diet?
Elimination diets are helpful for pinpointing problematic food, but it’s not meant to be a long-term diet. The beauty of a food sensitivity test is that it helps you identify which ingredients to hone in on, as opposed to a broader diet like FODMAPS which’s even more restrictive in terms of what you can’t eat.
After getting your food sensitivity results, you can go about the elimination diet in two ways:
- Focus on eliminating high or moderate reactivity foods (so class 3 and 2) and completely remove those ingredients from your diet for four weeks. This is a better option if you have a lot of ingredients on your list, as I did.
- Eliminate all class 1-3 foods from your diet for four weeks. In either case, you can ignore any ingredients you’re not reactive to in class 0.

The true magic happens with the add-back challenge: After four weeks, you begin reintroducing one food at a time (with just one serving of that food). Then, you don’t eat that ingredient for 2-4 days as you monitor your stomach symptoms. If you don’t have any symptoms, you can go back to eating that product like usual. Next, you repeat that step with different reactive food. It’s a time-consuming process, but worth it if you want to alleviate your stomach issues once and for all.
It’s important not to eliminate all your reactive foods forever. The goal is to add back as many foods as possible so you still have a healthy, balanced diet.
What if an elimination diet is too difficult?
I’ve always been stressed about doing an elimination diet since eating out and enjoying different types of food has always been one of my favorite parts of socializing. But now that I’m home 24/7 during the pandemic, it felt like it would be a missed opportunity not to finally give it a whirl without the social pressures of eating out or grabbing drinks with friends.
I decided that a phased elimination diet (where I only eliminated class 3 and 2 foods) was best for my current lifestyle and provided me enough food options that I could still enjoy.
The best tips for a successful elimination diet includes:
- Brainstorming about substitutions: For example, dairy-free coconut milk instead of cow’s milk.
- Keeping the fridge prepped: Many of the meals and snacks that I liked to eat on a regular basis contained my high reactive ingredients, so it was essential to have a stocked pantry with other options.
- Meal planning: Use a journal or notebook to figure out what your meals are going to be for that week so you don’t slip up.
- Cooking at home: It was too complicated to eat out or order take-out when you never know all the ingredients the restaurant is using and what kind of cross-contamination is happening behind the scenes.
An elimination diet is very, very difficult if you’re a food lover, like me. However, thanks to this food sensitivity test, it’s a lot more manageable when you can target specific foods instead of broader categories. And, the luxury of working from home during the pandemic made the elimination diet feel more feasible overall.
Still, I, unfortunately, gave up with my class 2 food elimination halfway through the month because it was too difficult to eliminate gluten. So far, all the gluten-free products I’ve tried just don’t do bread any justice! But I did learn some valuable information about how my body reacts to class 3 foods. I definitely felt less symptomatic with gastric issues by eliminating cow’s milk from my diet. Now that I’m past the add-back challenge, I avoid cow’s milk when possible, but I don’t drive myself crazy if a meal has some cow’s cheese. I learned that I could also live with a little bit of bloating if it meant I could enjoy an amazing croissant with brie. It really depends on how bad your stomach symptoms are and what you can live with — it’s all about striking the right balance.