What do Kim Kardashian, Cara Delevigne, Cyndi Lauper, LeAnn Rimes and Jonathan Van Ness have in common? They all have psoriasis.
Celebs, they’re just like us, right? In all seriousness, psoriasis is an autoimmune skin disease affecting over 125 million individuals worldwide. Yet, despite its prevalence, general awareness and understanding remain low, because it’s often confused with other skin conditions like dermatitis and eczema. This is particularly true for how the disease presents itself on darker skin: It took nearly nine months and two misdiagnoses for Diedre McClover, a doula who wrote an article titled “What It Means to Be a Black Woman Living with Psoriasis,” to get properly treated.
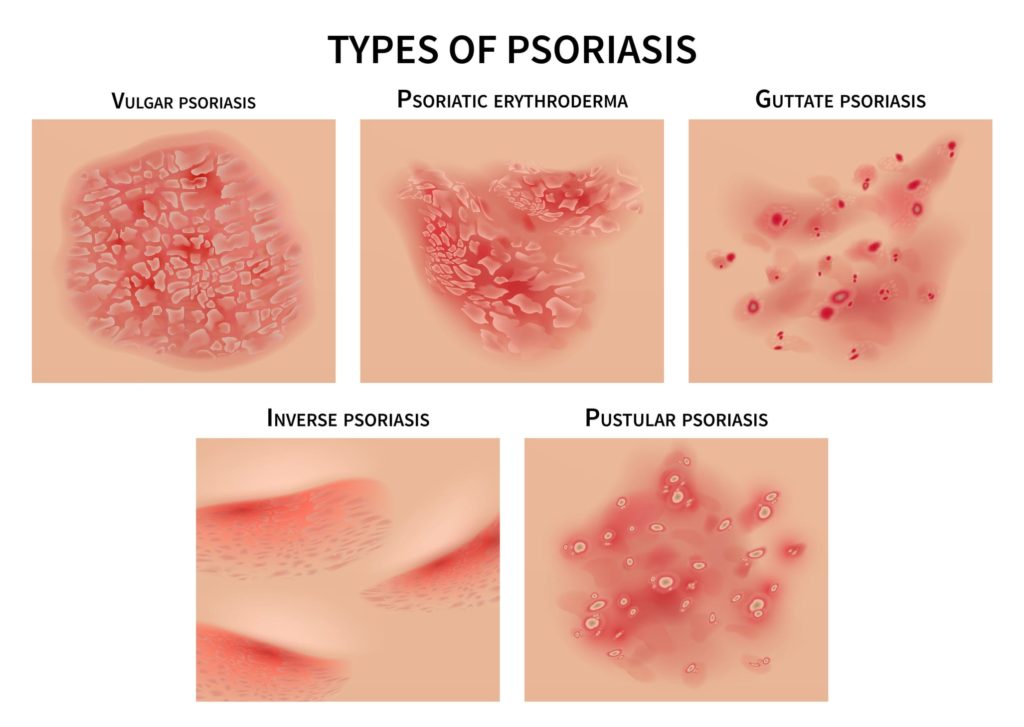
Although there are several types of psoriasis, they’re essentially “all variations on a theme,” explains Dr. Martin Wade, consultant dermatologist and medical director at London Real Skin. In short, psoriasis looks like large, red patches of scaly skin that can look inflamed, itch, and bleed from the cracking. “These can be itchy or sore but, despite what the myths say, psoriasis is not infectious,” says Wade.
It can appear pretty much anywhere on your skin:
- Plaque psoriasis: Also called psoriasis vulgaris, this is the most common form, which affects about 6.7 million adults in the U.S. alone, typically appears on your arms and legs, elbows and knees, and on your scalp.
- Guttate psoriasis: This involves a greater number of patches that are smaller in size. “It tends to be a bit more explosive, and can cover a lot of the body in a short period of time,” says Wade.

- Inverse psoriasis: This is sometimes referred to as hidden psoriasis because it’s found in your skin folds like in your groin, inner thigh, armpits, or under your breasts.
- Pustular psoriasis: These are scaly, pus-filled pustules and appear blister-like.
No, it’s not eczema
Thanks to its dry appearance, many confuse psoriasis with eczema – but there are notable differences. Psoriasis tends to occur on the outside of the elbows and knees, whereas eczema is more likely seen on the other side of these joints. It’s also found in areas where eczema doesn’t usually arise, such as the scalp.
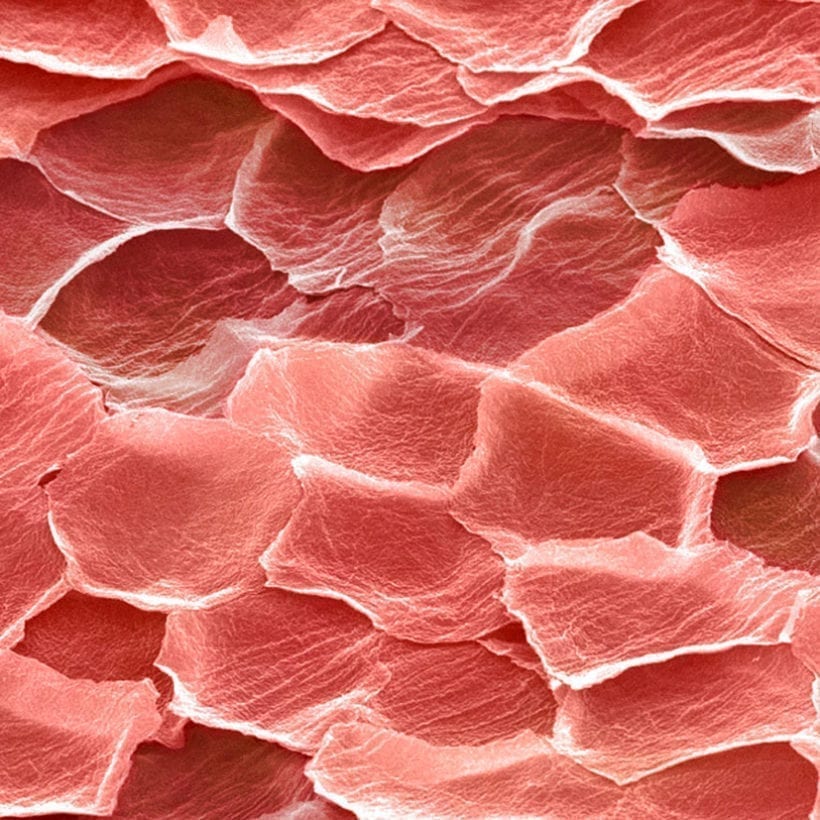
“It started on my scalp, which to this day is where the worst patches are during a flare-up,” says Jen Parker, book editor and designer. “Layers of skin flake off or crack and bleed, and it gets very red and very sore. Aside from my scalp, the biggest patches have been on my leg, and on my right foot. The toenails on my right foot also look like they have a serious fungal infection, and are very difficult to cut,” she says.
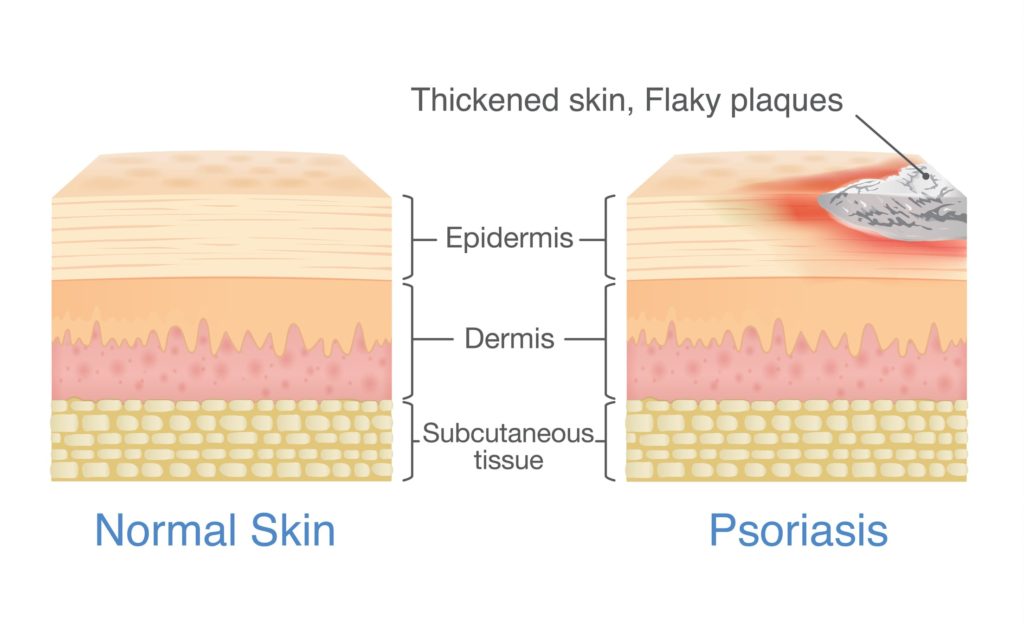
“We tend to see a well-demarcated plaque with psoriasis, which means you can see the edges of the lesion. With eczema, it often just fades out into nothing,” says Wade. “The redness with a silvery scale on top is also something we’d be looking for,” he notes, while inflamed patches of skin are thicker in psoriasis, too.

It’s also important to consider that psoriasis is associated with a number of other health concerns. “For years, we thought it was just a skin condition; but we’re now talking about metabolic syndrome,” Wade reveals. “People with psoriasis are more likely to have problems with their metabolism, and have cardiovascular disease.”
As many as one in three with psoriasis also develop joint pain, known as psoriatic arthritis. “This tends to affect the larger joints, such as the knee or elbow, but can also affect the hands,” he explains.
And then there’s the impact on mental health. “There’s a big psychological overlay,” says Wade. “Psoriasis can lead to depression and anxiety, and big changes to your daily life.” Indeed; many with psoriasis are highly self-conscious – only wearing particular clothes and avoiding places such as swimming pools.
More than skin deep
The all-important question: What causes it? As with many conditions, genetics come into play, but psoriasis isn’t classed as hereditary. “We call it ‘familial’,” says Wade. “There is a genetic basis, but it’s not as easy as saying that, if your dad’s got it and your mother hasn’t, there’s a 50 percent chance you’ll have it.”
While the location and appearance of psoriasis can vary, in all instances it results from a ramped-up inflammatory response in the body. “Psoriasis is considered a systemic condition,” he says. “The body’s own white blood cells are honing in and causing an inflammatory response in the skin.”
Psoriasis isn’t more prevalent in any particular gender or race and can occur at any age; although onset is most common in teenagers and young adults, which can be particularly tough when already dealing with the turbulence of puberty. The American Journal of Clinical Dermatology found that severe psoriasis happens more in men than women.
Skin saviors
While there is currently no cure, the good news is there are plenty of treatment options to help keep psoriasis under control – both medical and holistic.
Topical corticosteroid creams

These are the starting point, “especially if the psoriasis is limited to smaller areas,” says Wade. However, skin can become used to these, so a blend of two ingredients tends to be preferred. “We often use a combination that’s got a steroid and a vitamin D analog,” he adds.
Phototherapy
This works by using UV light to lower inflammation and slow production of skin cells, and is “a very safe treatment in the right hands,” Wade states. “A dermatologist would recommend this if the psoriasis is resistant or covering enough areas of skin.”
Prescriptions
Because psoriasis is well studied, you have options when it comes to medications. These can be administered through oral tablets or injections, but “we limit this to people who have got resistant or wide-spread psoriasis that we can’t control with topical therapy,” explains Wade. Bristol Myers Squibb, a global pharmaceutical company based in NYC, recently announced positive data from a new psoriasis drug trial, which saw at least a 75% improvement in patients with plaque psoriasis compared to a placebo.
Sunlight
“A lot of people notice their psoriasis gets better with sunlight, and over the summer months they might get some gentle sun exposure,” Wade notes. Although, this isn’t an excuse to book a sunbed appointment or skip sunscreen.
Lower stress
“We see psoriasis get a bit worse when people are stressed or anxious,” states Wade. However, although stress can exacerbate symptoms, it doesn’t cause them. Parker highlights stress as the primary cause of her flare-ups. “During the first COVID-19 lockdown, my psoriasis went crazy. Large flakes of skin were taking the hair with them as they came off.”
Your diet
Studies into the correlation between psoriasis and diet are thin on the ground, but – because this skin condition is an inflammatory disease – it’s thought eating foods that help control inflammation may help. Studies have shown that those who follow a Mediterranean diet of fish, whole grains, and fresh fruits/veggies had fewer psoriasis flare-ups.
Your skincare routine
If yours contain sodium lauryl sulfate (SLS), it’s time to find an alternative. “My dermatologist told me this is especially detrimental to psoriasis sufferers,” shares Parker. “It made a huge difference when I cut it out, especially from shampoo.”